Why this page
Our website is a platform that provides a glimpse into the function of brain barriers and our research projects in this field. As a dynamic webpage it is under constant development. If the content rises specific questions, or you would like to have more information on a specific topic, be very welcome to contact us!
Our aim is to advance the scientific understanding of brain barriers and by doing so, get one step closer toward helping patients suffering from brain diseases. We have developed this webpage, BrainBarriers4You, to introduce you to the brain barriers and to inform you about the range of projects within our BtRAIN consortium.
Introduction
Brain Barrier
Brain Barrier Introduction
Our brain is a very important organ so it needs to be protected. To do so, there are barriers defending it, like the walls of a castle. These barriers stop dangerous substances, like castle walls prevent enemies to enter, but at the same time they allow the passage of nutrients and the exit of waste. Hence, the barriers are very selective, but when they don’t function well, the brain can start developing a disease. It may also happen that the brain is sick and needs treatment. The problem though, is that the barriers protecting the brain may also prevent medication to cross, so the brain does not receive the treatment. It is as if, unfortunately, the guards at the walls of the castle cannot distinguish the people who want to help from the ones posing harm, and do not let any of them pass. This is why brain diseases like Alzheimer’s disease, multiple sclerosis and brain cancer are so difficult to treat, and why we urgently need to understand much better how the brain barriers work. Only then we will be able to design drugs and strategies to treat these diseases.
Contact
Please visit the official BtRAIN project website to get in contact with the ESRs or network members. http://www.btrain-2020.eu/
Why do we have brain barriers
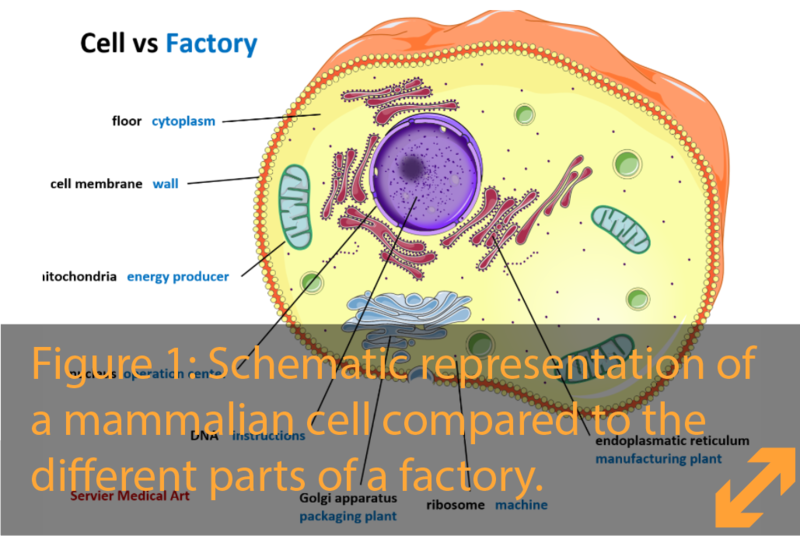
Our body consists of organs such as the liver, kidney, heart, lung, muscle and the brain which, like a well-oiled machine, intimately work together for us to breathe, run, think, laugh and dream, every day and every night. The central control for all this activity lays in our brain and spinal cord, which together we call the central nervous system (CNS). The CNS coordinates all the information it receives from our body and the environment surrounding us and gives back commands to our muscles to move, our lungs to breathe, our eyes to look and our mouth to eat and speak.
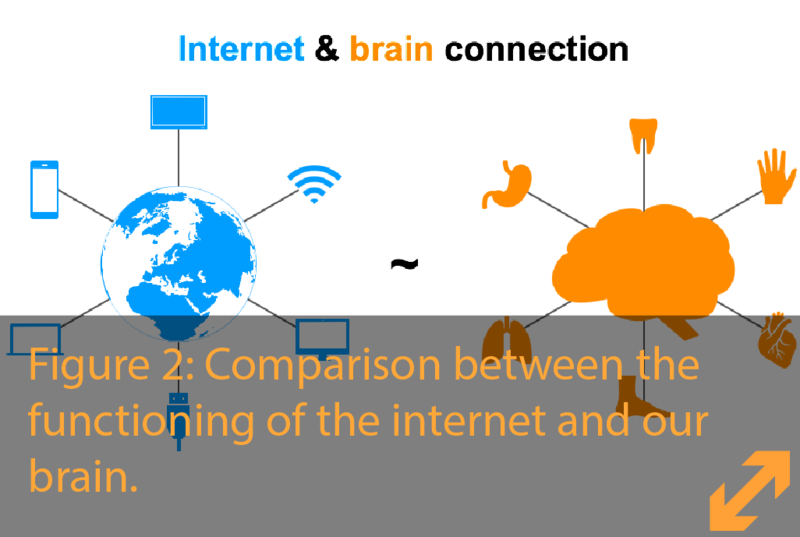
This exchange of information is performed by cells we call neurons that, like an internet network, form cables connecting all our organs and muscles to different organization centers in the brain and, in return from the brain, reach out to control the body.
For the activity of these neurons it is extremely important that the environment they are in (our brain) is kept constant without big changes and disturbances. The importance of this is illustrated in alcohol intoxication. Alcohol is an exceptional and small molecule that can easily cross the brain barriers.
When alcohol gets into the brain it alters the availability of nutrients and the stability of the neurons leading to the effects on our mental state that many people know. Imagine if everything we eat or drink could easily get from the blood into our brain, every day after a good lunch we would need a long time to recover! Our brain needs to be isolated from exposure to these substances that can change brain activity. In addition, our brain also needs protection against invasion by dangerous organisms, such as bacteria and fungi, as well as viruses that could destroy brain tissue. Therefore, the brain barriers allow the controlled entrance of nutrients in an ordered manner while blocking toxic substances or organisms that could harm our brain.
Did you know?
Alcohol is one of the special molecules that is able to cross the blood brain barrier. This is possible because it is soluble in fat. Another word for fat is lipids. Our cell membranes are formed by a double layer of these lipids similar to a soap-bubble, and are therefore characterized as being ‘lipophilic’ which means ‘to love lipids’.
Most molecules in the bloodstream are only soluble in water and cannot cross the ‘lipophilic’ cell membrane. These molecules are called ‘lipophobic’, meaning ‘fat-fearing’. However, molecules that are lipophilic, such as alcohol, can get into the brain. Another example is opioid painkillers such as tramadol. Luckily, tramadol is lipophilic and therefore can easily reach the central nervous system to decrease our perception of pain. Haloperidol, a classic antipsychotic, is another example of a lipophilic drug.
Lipophilicity versus lipophobicity is thus an important feature to take into account when developing drugs to treat brain diseases. At this moment, we still do not have the knowledge and tools to open the brain barrier in a safe and controlled manner. This is why drug treatment for brain diseases remains limited only to the use of molecules that are lipophilic.
⠀
This is why we need the specialized structures called ‘brain barriers’ that separate the brain from the rest of the body and, like a fortress, protect it against the entry of toxic substances and infectious agents. The brain barriers cannot be completely impenetrable, since in this case the brain would not receive nutrients and would starve. Therefore, the barriers are on one hand managing protection from the entry of unwanted material, but at the same time they have highly active transporters for nutrients and oxygen from the blood to the brain like a fortress has guarded gates, that can be opened for farmers to bring in supplies.
Did you know
As in the rest of the body, cells in the brain get old and die. This process of cellular death includes the neurons. In healthy ageing, we lose neurons as a natural process, but since we have enough remaining neurons to compensate, our brain function is unaffected. However, a disease can affect the brain by destroying neurons, a process known as neurodegeneration. This occurs in Alzheimer’s disease, where for reasons we still don't fully understand, unwanted material accumulates in our brain causing neuronal death. When too many neurons are lost, the effect on brain function becomes evident, as in Alzheimer’s disease by progressive memory loss.
Barriers
in our brain
The blood-brain barrier
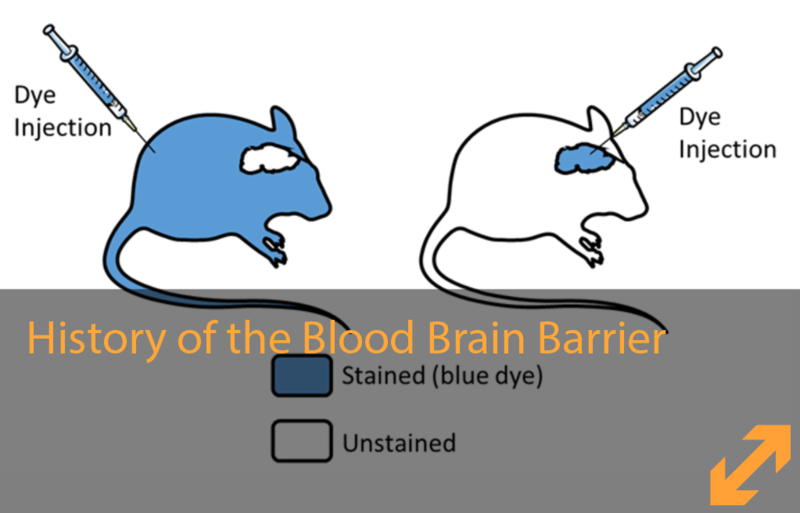
The blood-brain barrier (BBB) is a barrier that separates the brain from the blood.
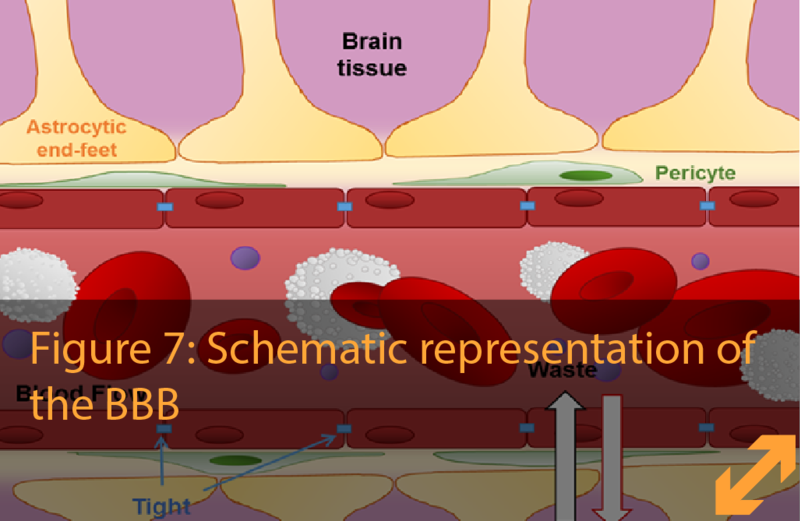
Our blood flows through a network of vessels in every organ in the body to carry essential nutrients and oxygen and remove waste products. The brain is a very dynamic organ and it needs a delicate equilibrium. On the other hand, harmful substances circulating in the blood must be prevented from getting into the brain and cause damage. Such harmful substances can be molecules like toxins, but also pathogens like bacteria or viruses. This dual regulation is possible due to the presence of the BBB, which is formed by a special kind of blood vessels: the brain capillaries. These capillaries are the smallest blood vessels in the brain and consist of thousands of cells placed along each other forming tubes. In addition, other types of cells participate in giving the BBB its barrier properties, which we explain below.
Did you know?
The brain capillaries are around 650 km long and have a total surface area of 20 m2.
1. Endothelial cells: the wall of the BBB
The endothelial cells are connected to form the wall of the blood vessels in our body. These cells have different characteristics depending on the organ. For example, the liver receives the blood from the heart, and functions to clean the blood and take-up and distribute all the nutrients from our digestion. The contacts (or junctions) between the endothelial cells are therefore very open, like a mesh, to absorb and process all this content from the blood. In contrast, in the brain, the junctions between the endothelial cells are very tightly sealed together.
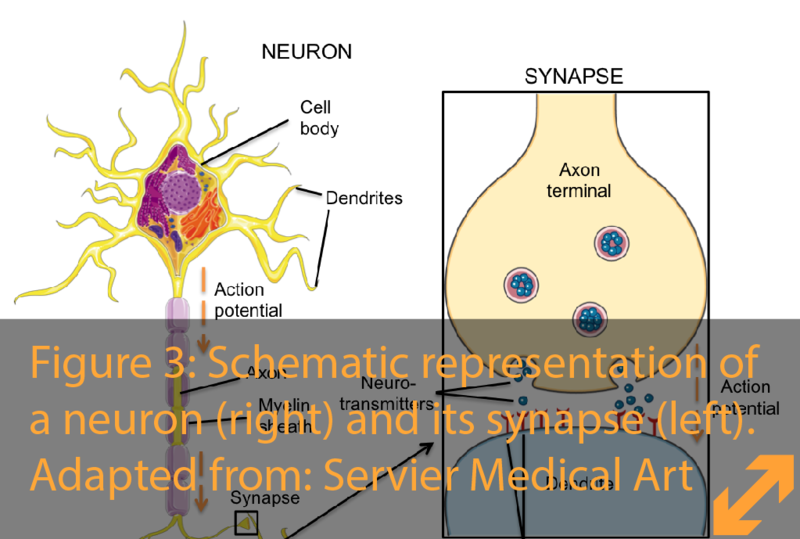
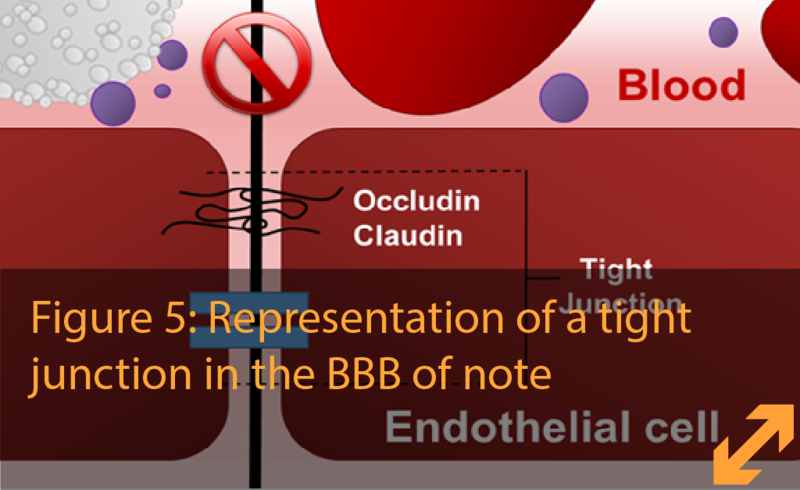
Junctions between endothelial cells are created by special molecules called cellular adhesion proteins. These proteins act as a zipper between the cells, allowing them to control the entry of substances by opening and closing the zipper. (Figure 5)
Did you know?
The information for building the complex and unique proteins is stored in our DNA. We therefore need a lot of information in our DNA. That is why if we aligned all the DNA of our cells it could encircle the earth almost 3 times!
There are different types of junctions that zip the endothelial cells together. One of these junctions are also present in endothelial cells outside of the brain. These junctions glue or adhere cells together keeping amongst others the red blood-cells from leaking out of the blood-vessels, and are called ‘adherens junctions’. Another important type of junctions present in endothelial cells are particularly strong in those of the BBB. When looked at very high magnification in the electron microscope, the cells appear to be firmly together, therefore, the junctions are called “tight junctions”. Tight junctions are also found in other cell types and tissues like liver and kidney and limit the free crossing of molecules and salts in-between cells. Consequently, these connections act as a true physical barrier, similar to the walls of a fortress. The way the endothelial cells transport essential nutrients across this barrier is by the use of special transporters that act like transport trucks. The endothelial cell would be similar to a logistic enterprise with trucks going from the blood to the cell and forth, and from the cell to the brain and forth. Also, when needed, the cell can keep the specific cargo of these trucks for its own use (such as iron, sugar, and salts). Thus, the tight junction is a closed road, like in former times the borders were barred, and crossing through the cell is strictly controlled by the 'logistics company' (figure 5).
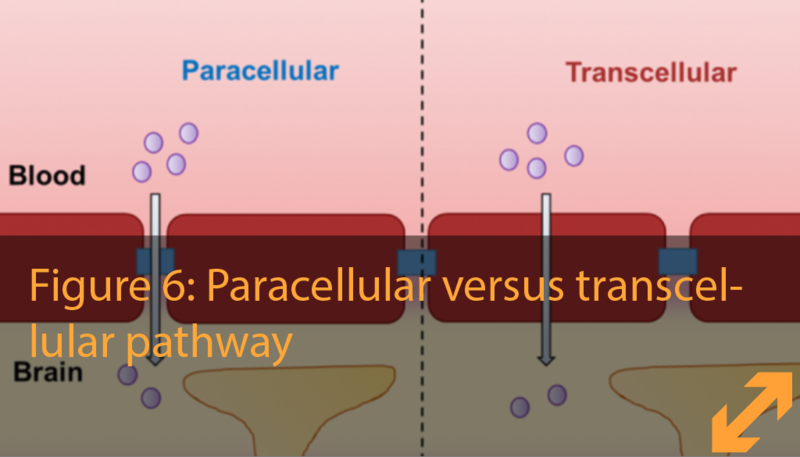
To reach the brain, molecules and cells have different pathways to cross the BBB: ‘in between the cell wall’ and “through the cell membrane’, known as paracellular and transcellular pathway. This is an important distinction to make when studying the leakiness and the movement of molecules or cells across the BBB.
Did you know?
Physical exercise enhances our memory and cognitive function. Studies have shown that physical exertion transiently opens the blood brain-barrier slightly. Some scientist argue that this would allow the passage of factors that stimulate the neurons in our memory-centre to grow, which aids in making our brain smarter.
2. Pericytes: an essential coverage
The word pericytes is derived from ‘peri’, which means around, and ‘cytes’, another word for cells. Pericytes are contractile cells that partially cover the capillaries by wrapping themselves around the endothelial cells like a sheet of ivy. By doing so, the pericytes fulfil their important role in shaping and stabilizing blood vessels. In the brain, these cells are essential for maintaining the BBB characteristics of the endothelial cells.
The way pericytes and endothelial cells are connected is through a special thin cover in between and around both cell-types called the basal membrane, which helps to glue the cells together. This close relation makes it possible for the pericytes to regulate the blood flow either by contracting the vessels and narrowing their diameter (vasoconstriction) –comparable to a tight handgrip around a hosepipe– or by loosening of this grip (vasodilation). This interaction also gives pericytes the ability to communicate with the endothelial cells to regulate endothelial leakiness (also called permeability).
When the pericytes don’t work properly, waste products can build up, leading to or worsening pathological conditions such as Alzheimer’s disease.
3. Astrocytes: an important support
The astrocytes are a special cell type of the so-called "glial cells" of the brain, providing support and protection to the neurons.
The brain consists of two main types of cells: neurons and glia. The term "glia" literally means "glue" or "filling" and it was given to this group of cells because it was initially thought that their function was to simply maintain the brain together. Glial cells support neurons and help maintaining the brain environment.
Glial cells can be subdivided in astrocytes, microglia (the immune cells of the brain) and oligodendrocytes (forming the insulating myelin sheath around the nerves).
Astrocytes are numerous and diverse in the brain. Their name means ‘star cells’ due to their star shape with many ramifications that allow them to reach both neurons and blood vessels.
The ramifications stretching out to the blood vessels finish in a specific shape which looks like a foot stepping on the surface of the vessel, and are therefore called astrocytic end-feet. These feet enable the astrocytes to act as mediators between the neurons and the blood. Thanks to these connections astrocytes can, for example, regulate the vasodilation and vasoconstriction (in a similar way to the pericytes) of the blood vessels, thus decreasing or increasing the blood-flow. In addition, astrocytes maintain the structure of the BBB by regulating the interaction between endothelial cells and pericytes, and stimulating the formation of endothelial tight junctions.
Did you know?
In diseases such as Alzheimer’s or epilepsy, where a lot of neurons are lost, astrocytes try to repair the tissue by increasing in number and changing their shape. This process is very similar to scar-formation but cannot replace the function of neurons.
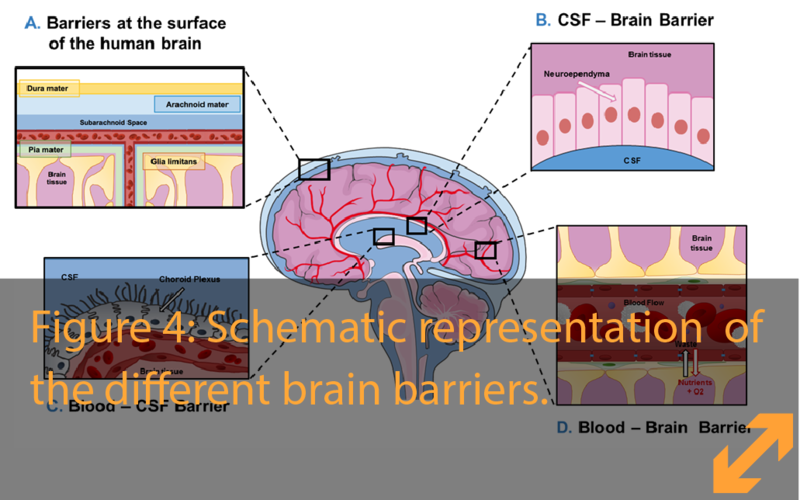
The blood-CSF barrier
Our brain is well protected from blows not only by the skull but also by a special fluid that surrounds it and flows in spaces in its center, acting like a cushion. This liquid, the cerebrospinal fluid (CSF), is produced by four special structures that are distributed within the brain. We call each of these structures the “choroid plexus” (Figure 4). They produce the CSF fluid by filtering water and nutrients from the blood into the space in which the brain floats.
The blood-vessels in the choroid plexus do not form a tight barrier and instead are loosely connected. In analogy to a fortress, those blood vessels have constantly opened gates without anyone controlling the passage of goods through them. However, there is yet another layer of specialized cells that tightly cover the whole choroid plexus, the so called epithelial cells. This layer of cells is in contact with the CSF on one side, and with the blood on the other, and pumps liquid and nutrients from the blood into the CSF.
Because the CSF is bathing the brain, it is very important that the epithelial layer of the choroid plexus remains tight and properly regulates what enters, similar to the endothelial cells in the BBB. This barrier in the choroid plexus is what we call the blood-CSF barrier. The blood-CSF barrier is a gatekeeper that keeps out harmful substances, while allowing the entry of necessary nutrients into the cerebrospinal fluid
Did you know?
The human brain is surrounded by 150 mL of CSF. Since it is constantly replaced, the brain needs to form half a litre every day, most of which is produced by the choroid plexus.
Did you know?
A vital function of the blood-CSF barrier is to protect the brain from infections. It does so by controlling the entry of specialized cells from the blood called immune cells, that like policemen patrol and check our cells to fight off infections and cells that behave out of the normal (for example cancerous cells). The importance of this surveillance is clear in brain infections: unfortunately, some viruses and bacteria are specially equipped to attack the brain and enter via the choroid plexus. When the patrolling immune cells fail to kill these so called pathogens they can infect the brain causing meningitis. The tight control of the entry of immune cells is also key for a healthy brain. In patients with Multiple Sclerosis (MS), some immune cells falsely recognize good cells of the brain as bad cells, and call out for help by sending out immune activating molecules. This triggers a chain reaction that enhances this auto-attack phenomenon ( ‘auto’ means ‘the self’, that’s why multiple sclerosis is classified as an ‘auto’-immune disease) and even more immune cells are recruited to the brain. This would be effective in fighting off infections, however in the end, these immune cells attack the brain tissue instead, leading to brain damage that cause the symptoms of the disease.
The CSF-Brain Interface
The inside of our brain contains four spaces, called ventricles, that are filled with CSF. At the interface between the CSF and the brain a barrier is created by a single layer of highly specialized epithelial cells also known as ependymal cells. This ependymal cell-layer does not form a complete barrier similar to the other barriers discussed, since it is full of gaps making it very leaky. This enables CSF to diffuse in and out of the brain. Of note, this is in contrast to the epithelial layer at the level of the choroid plexus where the CSF is produced, since here the epithelial cells touch the blood-vessels and form a the actual tight blood-CSF barrier. This leaky property of the CSF-Brain interface is very important for the CSF composition to be perfectly regulated.
Did you know?
The CSF-Brain barrier is probably the less studied among the brain barriers, nevertheless we know that it has very important functions that contribute to maintain a normal brain activity. For example, ependymal cells have particular structures called cilia, tiny hairlike structures (like your eyelashes, but in a cellular scale!) that beat in same direction, influencing the direction of the CSF and at the same time filtering out dangerous substances from it. Ependymal cells are not tightly connected between each other, this means that the CSF can pass into brain, allowing nutrients and other important substances to reach the neurons. Recent studies have shown that after stroke, ependymal cells can act like a sort of substitute soccer-players, “waiting” to be called in case of need. Indeed, after stroke for example, these cells can “enter the playfield” and transform themselves from ependymal cells into neurons, trying to ameliorate the damage caused by the stroke.
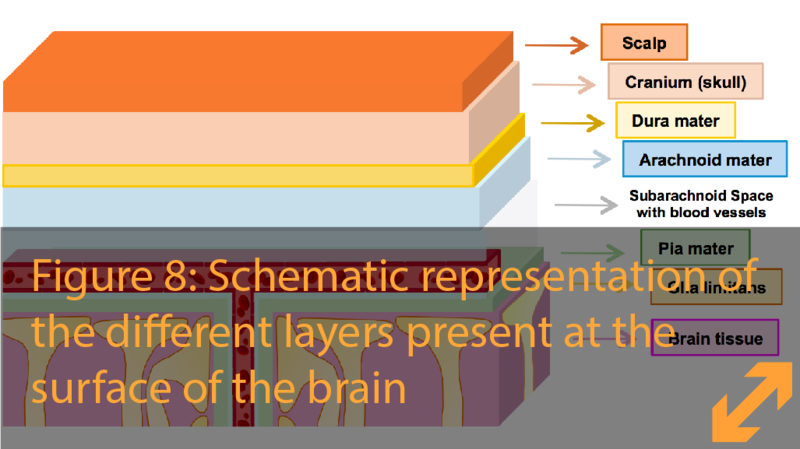
The barriers at the surface of the brain
Going from the scalp toward the brain, the first protection against traumas is the bony structure of the skull. Below the skull and before reaching the actual brain, we pass through the meninges, three layers that cover and protect the brain:
- Dura mater (latin for ‘hard mother’), the outer layer is covered by the bone and skin. This tough structure protects the brain and would hold everything together in case the skull brakes in an accident.
- Arachnoid mater (greek for ‘web-like’), the middle layer and first actual barrier before reaching the brain.
- Pia mater (latin for ‘tender mother’), the deepest layer of the meninges before reaching the first brain cells
There is a space between the arachnoid and the pia called subarachnoid space. This space is filled with cerebrospinal fluid, acting as a cushion to absorb shocks in the case of fast movements or traumas to the head.
To protect the entrance of harmful elements through the meninges, the cells of the arachnoid mater are tightly connected by tight junctions and isolate the brain similar to the BBB. Below the pia mater there is a layer of astrocytes called the glia limitans. There are no tight junctions between the cells of the glia limitans. This layer controls the trafficking of cells and molecules between the brain and the pia mater. Together, the layers of the meninges complete the brain's isolation from the rest of the body, thereby protecting it.
Did you know?
The mother of the brain
Early Arabic physicians called the meninges alumm al-dimagh, meaning the mother of the brain. This term was later literally translated into latin as mater.
Brain barriers: a dynamic field yet to be discovered
While the study of brain barriers started already over a century ago, ongoing discoveries and surprising findings indicate that our current knowledge touches only the tip of the iceberg! Technical advancements in biological research allow the investigation of BBB- characteristics, dynamics, and the cellular components in increasing resolution. The compound efforts and ongoing international data-sharing and collaborations among scientists over the past decades have been essential in the scientific advancement in this field. Two up-and-coming topics we are now able to address include the dynamic nature of the barriers, as well as the complex interaction between all the cells involved.
Brain barriers: a highly dynamic and changing structure
While in healthy conditions the brain barriers maintain a steady CNS, this does not mean the status quo of the barrier is static. Instead, the barriers are highly dynamic and actively maintained throughout life and adapt to different situations.
This becomes evident when, under certain conditions we all get exposed to, our brain barriers can become slightly leaky. For example, when we have a high fever, in altitude sickness or when performing extreme sports. This could partly explain why we experience a minor headache or confusion in these circumstances. This leakiness emphasises how dynamic the barriers are. Presumably, there is a need for this barrier to sometimes be more stringent and other moments more leaky, for reasons that are yet to be discovered.
The neurovascular unit: barrier formation through cooperation
All the cells in the neurovascular unit (endothelial cells, pericytes and astrocytes) interact and communicate in order to regulate the barrier properties.
Recent discoveries point out that the pericytes are essential for the transcellular transport across the BBB. Pericytes instruct the endothelial cells to acquire the specific transporting characteristics, as if pericytes were the CEO of the logistic BBB company controlling the trucks coming and going through the endothelial cells. Several studies are ongoing to better understand the way pericytes behave and can influence various diseases.
To complement, astrocytes regulate the tight junction integrity of the endothelial cells. While the importance of the astrocytes in tightening the endothelial cells was discovered already in 1987, only in 2011 scientists were able to identify the exact signaling molecule sent by the astrocytes to the endothelial cells instructing them to form these tight junctions.
Interestingly, the pericytes also help the astrocytes to find and surround the blood vessels with their endfeet. The close interdependence of these cells illustrates the critical role of the communication between all the cells involved to form a good blood brain barrier.
What is BtRAIN
BtRAIN projects
What is BtRAIN?
BtRAIN comes from merging the words "brain" and "to train". Our mission is to investigate all aspects of the brain barriers: from the early formation, the function and manipulation, towards the investigation of Alzheimer’s disease, multiple sclerosis, meningitis and ageing.
Brain disorders affect over a billion individuals worldwide, with around 300 million suffering from diseases such as brain cancer, multiple sclerosis, stroke, Alzheimer's and Parkinson’s. As our society is progressively aging, the number of brain diseases is expected only to increase. Current therapies provide mostly symptom relief and do not stop disease progression, highlighting the urgent need to better understand how the brain works and to develop novel strategies and treatments. Despite great advances in the understanding of the formation and function of the brain barriers, we still lack the knowledge to develop therapies for the diseases associated with dysfunctions of the brain barriers.
BtRAIN was created to bring together brain barriers researchers from different laboratories across Europe and collaborate in a joint effort towards dissecting the brain barriers functions and developing novel therapeutic interventions. The BtRAIN network is a European Training Network (ETN) from the Marie Sklodowska-Curie actions (MSCA). The latter provides research fellowship programmes that support PhD students (Early Stage Researchers, ESRs) by combining academic research with training by industrial partners. ESRs are given the opportunity to experience different sectors and develop transferable skills by working on joint research projects. The network includes 12 academic and non-academic partners, each hosting an ESR and several associated training partners. BtRAIN consists of 12 different projects, one executed by each ESR, which are interconnected by collaborations. Links to the individual projects can be found here: http://www.btrain-2020.eu/esrOverview
The BtRAIN projects
ESR 1 – Marjolein Heymans
In vitro models of the BBB and applications in pharmacological and toxicological screenings
In my individual project, I am testing different CNS drugs in vitro, which is a term meaning ‘in a test tube’ and is the opposite of in vivo, which basically means ‘in a living organism’. In my experiments, I make use of different types of human and animal cells, characteristic of the BBB, that are put together in such way that they mimic the BBB. This kind of experiments reduce the intensive and direct use of animals, but still gives us the opportunity to study the barrier mechanisms of the BBB. The main goal in this project would be to be able to use these kind of in vitro models to predict drug distribution into the human brain, as well as drug brain toxicity.
ESR 2 – Ana Raquel
In vitro models of the blood-brain and blood-CSF barriers using an integrated microfluidic device
The blood vessels are the part of the circulatory system that transports blood throughout the human body. Two important functions of the vessels are the separation and connection of the blood and the organs. The blood brain barrier (BBB) is a selective barrier that separates the circulating blood from the brain and nervous system. Due to the complexity of our brain, to treat several diseases ( like Alzheimer, Parkinson, cancer, etc) could be a real challenge. A cheap and easy way to experiment the BBB could be a model. Like an airplane model in the wind channel, the cells of the BBB can be cultured in a well-designed fluidic channel. In this model we can provide the physiological conditions and monitor the crucial parameters of the cells.
What could we do then? We can mimic some disorders of the system. We modulate the blood vessels of the brain to find better treatments. It is very important to get new tools to improve studies in real time.
ESR 3 – Raoul F.V. Germano
Comparison of mouse and zebrafish cerebral endothelial cell transcriptomes and functional investigation of conserved pathways governing brain angiogenesis and BBB formation
Despite the vital role of the endothelial brain barrier for adequate brain functioning, detailed knowledge on how formation of these blood-vessels is instructed remains lacking. To unravel novel genes involved in generating the endothelial barrier we take advantage of the zebrafish. This animal model provides the opportunity to, in living embryos, visualize and manipulate the development of the blood-vessels and their barrier-properties. In order to find genes that are essential for brain barrier formation we look at genes active in the BBB endothelium that are present in both the zebrafish and mouse brain vasculature. The idea is that as we vertebrates changed over the course of evolution from fish to mammals (mammals including us humans as well as mice), genes fundamental for BBB formation would have been maintained in the process of natural selection. Thus, comparing both species allows us to identify ‘core’ genes regulating endothelial acquisition of barrier properties and then select candidate genes to study in further detail. Understanding the function of these candidate genes would enhance our understanding of diseases affecting the brain, and provide opportunities to develop alternative strategies to treat patients suffering from these illnesses
ESR 4 – David M. F. Francisco
Integrative meta-analysis of public and novel vertebrate BBB omics data and establishment of the BBBHub platform
Information is important. However, for information to be useful it needs to be understandable and accessible. The main objective of my project is to find ways to expand the information we have about gene expression (transcriptome) on the Brain Barriers. For this I’ll be collaborating with other member of the network, analysing the expression data they will produce. I’ll also establish methodologies to compare existing data both in terms of the results but also of the quality. The end result will be a web platform where all the information regarding gene expression in the brain barriers will be collected and analyzed, allowing scientists in the field to better access, analyse and compare these datasets.
ESR 5 – Kakogiannos Nikolaos
The role of G-protein-coupled receptor Gpr126 signalling in the development of the blood-brain barrier
The complexity of the blood-brain barrier (BBB) has hampered efforts for drug delivery to the brain for the treatment of various pathological conditions, like cancers and neurodegenerative diseases. To this end, we need to understand the dynamics and molecular mechanisms that drive BBB formation through the identification of new genes. In our laboratory we have focused on a novel gene, Gpr126, which we believe to be important for the development of the BBB. We are trying to describe the role and the molecular mechanism of Gpr126 during the establishment of the BBB.
ESR 6 – Eduardo Frías-Anaya
Age-induced changes in gene and microRNA expression at the mouse blood-brain barrier
We all change during ageing, it is a natural and unstoppable process that affects our body and its several functions. As well as other organs, our brain gets changed as we age and it suffers different effects which will alter our cognition, memory or will make us more susceptible to neurodegenerative diseases but also vascular incidents (i.e. stroke). Neurovascular incidents are closely related to the blood-brain barrier (BBB), since during ageing the function and structure of this barrier gets altered and it becomes leaky, promoting the passage of components from the blood flow into the brain. These changes at the level of the BBB seem to be associated with changes in the expression of several genes and miRNA (small molecules that can promote or block the expression of many genes). We are trying to study which potential changes in expression at the blood brain barrier can correlate with the structural and functional alterations observed in ageing.
ESR 7 – Ricardo M. Figueiredo
Blood-brain barrier derived non-coding RNAs as functional biomarkers for the aging BBB versus the BBB in Alzheimer’s Disease
Being Alzheimer’s Disease (AD) one of the most prevalent dementia seen in elderly worldwide affecting almost 13.8 million people around the globe, it’s urgent the finding of accurate and noninvasive diagnosis and prognosis methods. Currently, the preliminary diagnosis of AD is made by a combination of clinical criteria which includes a neurological examination, mental status tests and brain imaging. However, based on the above clinical tests, the diagnosis of AD becomes difficult especially in patients having mild or early stages of AD. Since the properties of the blood-brain barrier (BBB) are altered in the brains of AD patients, we expect endothelial cells to express different genes in this condition. Consequently, different small RNA molecules might be released to the blood of AD patients. For that reason, we will develop sensitive techniques to analyse the blood and find small RNA molecules with origin in the dysfunction of the BBB. If the small RNA molecules found in the blood are the same found dysregulated in BBB’s endothelial cells, we can use these molecules as functional biomarkers for this condition. These RNA molecules might be used in the future for AD diagnosis.
ESR 8 – Luca Marchetti
Brain endothelial mechanisms directing the cellular pathway of T cell migration across the BBB
The function of immune cells is to protect us from infections and external agents. However, during autoimmune diseases, in conditions not fully understood, immune cells can become harmful for ourselves and attack our own body. During multiple sclerosis, an autoimmune disease of the central nervous system, immune cells can cross the BBB and cause damages in the brain. In my project we try to understand the differences between the mechanisms used by two particular types of immune cells to cross the BBB, namely Th1 and Th17 T cells. Furthermore, we know that T cells have two possible pathways to cross the BBB: ‘in between the cell membrane’ and “through the cell membrane’, known as paracellular and transcellular pathway. In our lab, we can stimulate the endothelial cells of the BBB with conditions that direct the T cells preferentially to trans or paracellular. By using a modern technique (RNA sequencing) that allow us to have a full view on which genes are active in the endothelial cells of the BBB in those conditions, we aim to identify which of those genes are able to direct the T cells to trans or paracellular pathway. Both approaches will help us to have a better understanding of how T cells can cross the BBB during multiple sclerosis. By identifying which genes are crucial in this process, we aim to ameliorate the current treatments for multiple sclerosis, enhancing the specificity and reducing the side effects of the treatments.
ESR 9 – Amaia Dominguez-Belloso
Contribution of the BBB in amyloid-β biology in Alzheimer’s disease
Amyloid-β (Aβ) is one of the 2 main molecules accumulating in the brain of Alzheimer's disease (AD) patients, destroying the neurons and leading to the symptomatology of memory loss that we all know. BACE-1 is the name of the molecule generating Aβ. Our lab previously showed that the endothelial cells (ECs) of the brain vessels contain active BACE-1, which could potentially contribute to AD. Our aim is to understand the role of the ECs in AD, and we hope to discover new therapeutic targets such as BACE-1 in ECs to treat this terrible disease that affects an ever increasing part of the population in western countries.
ESR 10 – Markus Schuster
Exploring CD4+ T cells as carriers to mediate transport of drugs across the blood-brain barrier
Our aim is to develop a drug shuttle system that can be used to facilitate the transport of drug molecules from the blood to the brain. Therefore, drugs are encapsulated into small polymeric nano-capsules called polymersomes, that are formed by the use of biocompatible and biodegradable polymers. To deliver those polymersomes across the BBB to the brain, the polymersomes are conjugated to T-cells that have the innate ability to cross the BBB and naturally home in the brain parenchyma. After the T-cells have carried the polymersomes to their final target, the polymersomes undergo degradation by time until they detach from the cells and release their cargo.
ESR 11 – Marie Wiatr
Role of differnet receptors in promoting pathogen and leukocyte migration across the BCSFB in meningitis
My project is about how a virus can cross the brain barrier and enter the brain. I am working on a specific virus that causes meningitis, echovirus 30. This virus causes the disruption of the brain barrier and can damage the brain. I am trying to identify how the virus can enter into the epithelial cells of the brain barrier, and by which mechanism and which molecules the virus is attaching to penetrate inside the cells.
When you are sick, specific cells, the immune cells, are fighting against the pathogens. Another part of my work is to identify how these immune cells enter in the brain when there is an infection.
ESR 12 – Sabela Rodríguez Lorenzo
Molecular control of the human brain barriers in health and neuroinflammation
To maintain the delicate environment in the brain, the cerebrospinal fluid (CSF) that bathes the brain is separated from the blood by the blood-CSF barrier in the choroid plexus. This barrier is a gatekeeper that prevents the entry of harmful substances. In multiple sclerosis (MS), the cells of the immune system, which usually protect the body against external threats, can enter the brain and attack the myelin sheath that surrounds the neurons.
We want to understand what goes wrong in the blood-CSF barrier in MS. We used a technique called “RNA-sequencing” to compare the gene expression profiles in the choroid plexus from MS patients and healthy donors. Studying the altered genes in the choroid plexus of these human samples will help us understand the mechanisms that contribute to blood-CSF barrier functioning and hopefully, in the future, they could be used as drug targets to treat MS.
Videos
BBB related